In patients with low-risk cervical cancer, simple hysterectomy has demonstrated noninferior pelvic recurrence rate at 3 years and lower rates of surgery-related urologic adverse events (AEs) vs radical hysterectomy in the phase III, randomized, noninferiority CX.5 SHAPE trial.
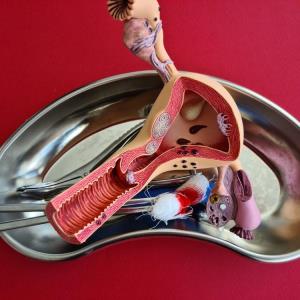
The trial included 700 patients recruited from 130 centres in 12 countries between December 2012 and November 2019. Most patients (91.7 percent) had stage IB1 disease according to the 2009 International Federation of Gynecology and Obstetrics (FIGO) criteria. More than half had squamous-cell carcinoma (61.7 percent) and histologic grade 1 or 2 tumours (59.3 percent). The patients were randomized to undergo simple hysterectomy (n=350; median age, 42 years) or radical hysterectomy (n=350; median age, 45 years) with lymph-node assessment. The choice of open vs minimally invasive approach was at the discretion of participating surgeons. [N Engl J Med 2024;390:819-829]
“With a median follow-up of 4.5 years, the incidence of pelvic recurrence at 3 years [primary outcome] was 2.52 percent in the simple hysterectomy group vs 2.17 percent in the radical hysterectomy group. The between-group difference was 0.35 percent [90 percent confidence interval (CI), -1.62 to 2.32], with the upper limit of the CI below the prespecified noninferiority margin of 4 percent,” the investigators reported.
Among patients who underwent simple hysterectomy, pelvic recurrence occurred in 3.2 percent (n=9/281) of those who underwent minimally invasive surgery (MIS) and 3.5 percent (n=2/57) of those who underwent open surgery. Among patients who underwent radical hysterectomy, pelvic recurrence rates were 2.9 percent (n=7/243) and 3.0 percent (n=3/99) for those who underwent MIS and open surgery, respectively. “However, the trial was not designed to address the safety of MIS in patients with low-risk cervical cancer,” the investigators pointed out.
Intraoperative surgical complications occurred in 7.1 percent (n=24/338) of patients who underwent simple hysterectomy vs 6.4 percent (n=22/344) of those who underwent radical hysterectomy. Bladder injuries occurred in 0.9 percent (n=3/338) vs 2.6 percent (n=9/344) and ureteral injuries occurred in 0.9 (n=3/338) percent vs 1.5 percent (n=5/344) of patients who underwent the respective assigned procedures.
“The incidence of surgery-related AEs was lower in the simple vs radical hysterectomy group within 4 weeks after surgery [42.6 percent vs 50.6 percent; p=0.04],” the investigators noted.
In particular, the incidence of urinary incontinence and urinary retention was significantly lower in the simple vs radical hysterectomy group, both within 4 weeks (urinary incontinence: 2.4 percent vs 5.5 percent; p=0.048) (urinary retention: 0.6 percent vs 11.0 percent; p<0.001) and beyond 4 weeks after surgery (urinary incontinence: 4.7 percent vs 11.0 percent; p=0.003) (urinary retention: 0.6 percent vs 9.9 percent; p<0.001).
Patient-reported quality-of-life and sexual function measures also appeared to favour simple vs radical hysterectomy overall.
For patients with early-stage cervical cancer, current guidelines of the National Comprehensive Cancer Network (NCCN) recommend open radical hysterectomy with bilateral pelvic lymphadenectomy. [NCCN guidelines: cervical cancer version 1.2023]
“Findings of this study challenge our current standards and provide evidence that simple hysterectomy, in selected patients, appears to be safe, yielding oncologic outcomes similar to those of radical hysterectomy,” wrote Dr Pedro T. Ramirez of Houston Methodist Hospital Neal cancer Center, Houston, US, in an accompanying editorial. “Accurate estimation of tumour size and depth of invasion with the use of preoperative imaging is critical for selecting patients with disease appropriate for conservative management.” [N Engl J Med 2024;390:861-862]
“Patients who do not meet such inclusion criteria [for simple hysterectomy] should continue to be offered radical hysterectomy,” Ramirez added.